SFC news published since 2018. See SFC archived content for earlier news articles.
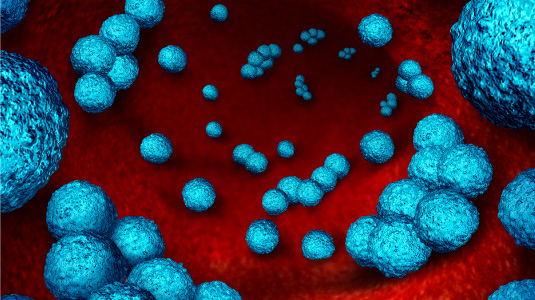
Is an antimicrobial resistance Armageddon upon us? Professor Mike Barrett, SULSA Director, shows how Scotland’s universities are leading the way in addressing the antimicrobial resistance challenge.

Scary predictions are that by 2050 up to 10 million deaths globally may be caused by antimicrobial resistant infections.
Scotland is a global leader in combating microbial disease and this April (26 and 27) the Scottish Universities Life Sciences Alliance (SULSA) is hosting a symposium at the University of Strathclyde to probe some of the big issues.
Average life expectancy is now twice what it was just 100 years ago when diseases like tuberculosis, typhoid, cholera, pneumonia and sepsis accounted for around half of all deaths. That all changed in 1928 thanks to a serendipitous discovery by a young Scottish doctor. In the summer of 1928 Alexander Fleming went on holiday and accidentally left behind an open plate of bacteria. Returning to work, he found that a fungus growing on the plate had killed the bacteria. He realised that the fungus was secreting a toxin which he called penicillin.
 Fleming’s discovery was the second great Scottish contribution to the war against microbes – in the nineteenth Century, Joseph Lister, then Professor of medicine at Glasgow University, introduced the concept of antisepsis, sterilising instruments used in surgery to prevent the spread of germs.
Fleming’s discovery was the second great Scottish contribution to the war against microbes – in the nineteenth Century, Joseph Lister, then Professor of medicine at Glasgow University, introduced the concept of antisepsis, sterilising instruments used in surgery to prevent the spread of germs.
The success of penicillin, a natural product made by one bug to kill others, stimulated an era of “bioprospecting” for other antimicrobial agents from bugs in soil. The post-war period saw a great expansion in the development of new antibiotics. It appeared that humanity’s battle against microbial infection would soon be won. However, mankind gradually began to take these wonder-drugs for granted.
They were given out inappropriately, for example to people with viral infections that won’t respond to antibiotics, which target only bacterial infections. Farmers started feeding antibiotics to animals, not because they were sick, but to promote faster growth and to combat their unsanitary living conditions. All animals (including humans) naturally harbour trillions of bacteria which share our food, hence killing them means we gain more energy from what we eat. The more antibiotics were given out, the higher the chances that resistance would arise. In recent years this problem has grown.
In the meantime pharmaceutical companies have turned away from antibiotics, because of the lack of return of investment. New antibiotics are not reaching the market because their efficacy can’t be shown, and they may not be better than existing antibiotics, meaning they can’t be licenced. A crisis is upon us. Infections generally thought of as trivial may become life-threatening again. Resistance to current antibiotics is already here and new drugs against bacteria are proving hard to find.
Scotland’s universities are leading the way in addressing the antimicrobial resistance challenge. Potential new drugs are being invented and new ways of diagnosing the problem are being developed. Leading physicians are calling for changes in policies to help combat the resistance that has surfaced, and several innovative companies have emerged to bring new products to the market place.
The SULSA symposium on antimicrobial resistance will span two days. On day one, leading scientists will present ground-breaking new research that is helping combat the problem. On day two, influential policy makers, including Scotland’s Cabinet Secretary for Health and Sport, Shona Robison MSP, will outline plans to intervene in this crisis. In addition to scientists, the public and journalists are welcome to attend.
Further information on the Antimicrobial Resistance Conference is available on the SULSA website.

